
12 Surprising Health Deficiencies in Texas Nursing Homes
Nursing homes are designed to be a place of comfort and care. A place where the ailing or elderly can get the attention and skilled care they need. Sadly, health deficiencies in Texas nursing homes,…
Nursing homes are designed to be a place of comfort and care. A place where the ailing or elderly can get the attention and skilled care they need. Sadly, health deficiencies in Texas nursing homes, and in nursing homes across the United States are putting residents at risk for illness, injury, or death. At MedMalFirm.com, our Houston nursing home abuse attorneys know all too well that Texas nursing homes are no exception.
Each year, the Centers for Medicare and Medicaid Services (CMS) compiles datasets outlining health deficiencies in nursing homes. The deficiencies are noted and scored, and can then be compared to other state and national averages. The most recent dataset suggests that in 2017-2018 there were 12 surprising health deficiencies in Texas nursing homes.
Health Deficiencies in Texas Nursing Homes
If you look at the graph below, the “other” category certainly stands out. But looks can be deceiving. While 67 percent of health deficiencies reported by Medicare are classified in the other category, the other 12 categories are really the surprising, and more dangerous, pieces of the pie. These 12 categories represent 12 surprising health deficiencies in Texas nursing homes that families should be aware of.
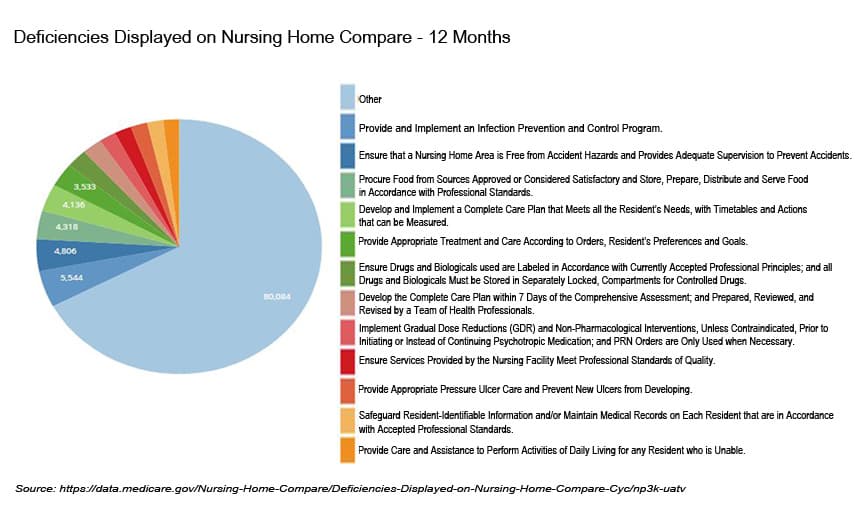
These 12 categories indicate the individual health deficiencies with a high enough percentage to warrant their own categories. The frequency and percentage suggests that these 12 deficiencies may be a consistent and ongoing problem.
1. Provide and Implement an Infection Prevention and Control Program.
Infection prevention and control programs are incredibly important in any healthcare setting. The Centers for Disease Control and Prevention (CDC) outlines specific guidelines for infection prevention and control in long-term care facilities. Unfortunately, data from Medicare suggests that many Texas nursing homes are not properly implementing such programs. Around five percent of health deficiencies in Texas nursing homes were related to infection prevention and control programs. That five percent accounts for 5,544 individual deficiencies.
2. Ensure that a Nursing Home Area is Free from Accident Hazards and Provides Adequate Supervision to Prevent Accidents.
Nursing homes must maintain an environment that is safe and free from hazards in order to prevent accidents, falls, and other injuries. Facilities must also be properly staffed to provide supervision and care for residents. Between 2017 and 2018, Medicare reported 4,806 deficiencies across Texas nursing homes related to accident hazards and adequate supervision. Those deficiencies made up four percent of all health deficiencies reported.
3. Procure Food from Sources Approved or Considered Satisfactory and Store, Prepare, Distribute and Serve Food in Accordance with Professional Standards.
Nutrition is a necessity for daily living. In healthcare settings, proper nutrition is even more important to ensure that residents are healthy. Nursing homes are required to follow guidelines related to food safety, including how food is stored, prepared, and served. When they fail to follow guidelines, they put resident safety and health at risk. According to Medicare data, in 2017-2018 four percent of health deficiencies reported in Texas nursing homes were related to food safety and compliance with standards. There were a total of 4,318 deficiencies reported across the state.
4. Develop and Implement a Complete Care Plan that Meets all the Resident’s Needs, with Timetables and Actions that can be Measured.
In nursing homes, a care plan is the foundation to ensuring that residents get the care they really need. Care plans are individualized plans created by staff, healthcare providers, the resident, and sometimes family members. The plan outlines the services that are needed, any equipment or supplies needed, dietary needs, healthcare needs, and goals. Nursing homes are required to develop and implement care plans in accordance with standards.
Sadly, that does not always happen as it should. During 2017 and 2018, Medicare reported a total of 4,136 deficiencies in Texas nursing homes related to care plan development and implementation. These deficiencies accounted for three percent of all health deficiencies reported in nursing homes during that time.
5. Provide Appropriate Treatment and Care According to Orders, Resident’s Preferences and Goals.
Once a care plan has been established, the nursing home must provide care and treatment based on that plan, any orders, the residents needs and preferences, and the residents healthcare needs or goals. It is the responsibility of the nursing home to ensure that each resident gets appropriate care and treatment, and that staff are capable of doing so. Failing to provide appropriate treatment and care is considered a health deficiency by Medicare. In 2017-2018, Medicare reported 3,533 deficiencies across Texas nursing homes, accounting for three percent of all deficiencies reported.
6. Ensure Drugs and Biologicals used in the Facility are Labeled in Accordance with Currently Accepted Professional Principles; and all Drugs and Biologicals Must be Stored in Locked Compartments, Separately Locked, Compartments for Controlled Drugs.
There are state and federal regulations related to storage of drugs and biological products in long-term care facilities, including nursing homes. CMS specifically has guidelines for how drugs are ordered, stored, managed, and administered to residents. These regulations are designed to promote safety and reduce medication errors. Among Texas nursing homes, deficiencies related to drugs and biological were noted in 2017-2018 with 2,825 deficiencies reported across Texas. Those deficiencies equate to two percent of health deficiencies reported.
7. Develop the Complete Care Plan within 7 Days of the Comprehensive Assessment; and Prepared, Reviewed, and Revised by a Team of Health Professionals.
In the past few years, CMS has revised their regulations related to how quickly nursing homes have to develop care plans and have them implemented. Nursing homes are now required to complete develop care plans within seven days of completing the comprehensive assessment (the assessment completed at the time the resident is admitted). One of the primary reasons for having a care plan developed so quickly is to ensure that residents get the care and treatment they need as soon as they move into the facility.
Even though CMS has specific guidelines, some facilities fail to complete assessments and care plans within established guidelines. Such failures are considered health deficiencies, which are measured by Medicare. Among Texas nursing homes, in 2017 and 2018, there were 2,677 such deficiencies. These deficiencies accounted for around two percent of all health deficiencies in Texas nursing homes during that time.
8. Implement Gradual Dose Reductions (GDR) and Non-Pharmacological Interventions, Unless Contraindicated, Prior to Initiating or Instead of Continuing Psychotropic Medication; and PRN Orders for Psychotropic Medications are Only Used when the Medication is Necessary.
Use of psychotropic medications as a form of “chemical restraint” have been a hot topic in the medical and legal communities in recent years. Many nursing homes in the U.S. have been found to use psychotropic medications as a way of managing residents deemed “difficult”, agitated, or who exhibited behavioral problems. There are many ethical concerns with using these drugs outside of their U.S. Food and Drug Administration (FDA) designations. In fact, the FDA has issued a black box warning about psychotropic medication use, which has propelled CMS to expand oversight.
Sadly, use of psychotropic medications is still a concern in many nursing homes. From 2017 to 2018, there were a number of health deficiencies in Texas nursing homes related to psychotropic medications. Around two percent of health deficiencies – or 2,302 reports – were related to GDR and PRN use of psychotropic medications.
9. Ensure Services Provided by the Nursing Facility Meet Professional Standards of Quality.
CMS guidelines state that nursing homes must ensure that all services provided meet professional standards of quality and accepted standards of clinical practice. As CMS completes surveys of facilities participating in Medicare and Medicaid funding programs, they look for facilities to meet certain criteria. Criteria include ensuring that care plans reflect the standards of practice, that all standards referenced are up to date and accurate, and that the facility is compliant with CMS regulations.
Facilities who fail to meet the standards of quality or practice may be cited for health deficiencies related to these areas. Health deficiencies in Texas nursing homes related to the professional standards of quality and practice totaled 2,279 in 2017-2018. These deficiencies accounted for two percent of health deficiencies reported across Texas nursing homes.
10. Provide Appropriate Pressure Ulcer Care and Prevent New Ulcers from Developing.
CMS guidelines state that nursing homes must conduct a comprehensive assessment of every resident. Part of that assessment is reviewing a resident’s health and risk factors related to pressure ulcers, or bedsores. Based on the comprehensive assessment, facilities must ensure that residents who enter the facility without bedsores do not develop them, and that residents who do have a bedsore or who develop one get appropriate treatment. Preventing bedsores is the ultimate goal, but CMS also has guidelines for residents who have a bedsore, including treatment and prevention of new sores. Other related guidelines include infection control and wound care.
Health deficiencies in Texas nursing homes related to bedsores are a tremendous concern for patients and their families. Between 2017 and 2018, Medicare reported 2,257 health deficiencies across Texas nursing homes related to prevention or care of bedsores. That number represents two percent of health deficiencies in nursing homes across the state.
11. Safeguard Resident-Identifiable Information and/or Maintain Medical Records on Each Resident that are in Accordance with Accepted Professional Standards.
Nursing home residents must provide personal and identifiable information to administrators when they move in. It is incredibly important that this information is protected. Identity theft and financial exploitation are two forms of nursing home abuse or neglect that affect thousands of residents every year. Nursing homes are required to maintain identifiable information and medical records in a way that protects residents and meets accepted professional standards.
Sadly, many nursing homes fail to properly maintain records and protect resident information. In Texas, Medicare data from 2017-2018 indicates 2,166 health deficiencies in Texas nursing homes related to resident-identifiable information or medical records. These reports equate to two percent of health deficiencies reported over those two years.
12. Provide Care and Assistance to Perform Activities of Daily Living for any Resident who is Unable.
One of the primary reasons why nursing homes exist is to help individuals who need skilled care or have specific needs. Within that scope, it would seem only natural that nursing homes provide care and assistance and help residents perform activities of daily living. Nursing homes help residents maintain a clean, safe, and private environment. They help them with matters of hygiene, nutrition, exercise, and medical care. Many facilities also offer social events and outings.
Facilities participating in Medicare and Medicaid funding programs are monitored and surveyed routinely to ensure that they meet standards related to care and assistance with activities of daily living. In 2017 and 2018, there were 2,145 health deficiencies in Texas nursing homes related to facility failures in this regard. These reports accounted for two percent of health deficiencies noted.
What Data on Health Deficiencies Really Means
In order to protect nursing home residents and ensure that they get the quality care they need and deserve, state and federal agencies have created guidelines that nursing homes must follow. Furthermore, agencies routinely visit facilities and conduct surveys to see how nursing homes are performing, and whether there are any health deficiencies or compliance failures.
It is important to track health deficiencies so that governing agencies can work with nursing homes to correct problems before they get out of hand. Some nursing homes will quickly develop a plan of action for correcting deficiencies and ensuring that their residents are safe. Sadly, others continually ignore deficiencies or allow problems to escalate.
Nursing home residents should never suffer from a lack of quality or safety because of deficiencies in guidelines that are clearly stated and should be monitored. Facilities that fail to comply or continually fail to correct deficiencies must be held accountable.
